How Digoxin produces ventricular arrhythmias?
by egpat Posted on 10-06-2017
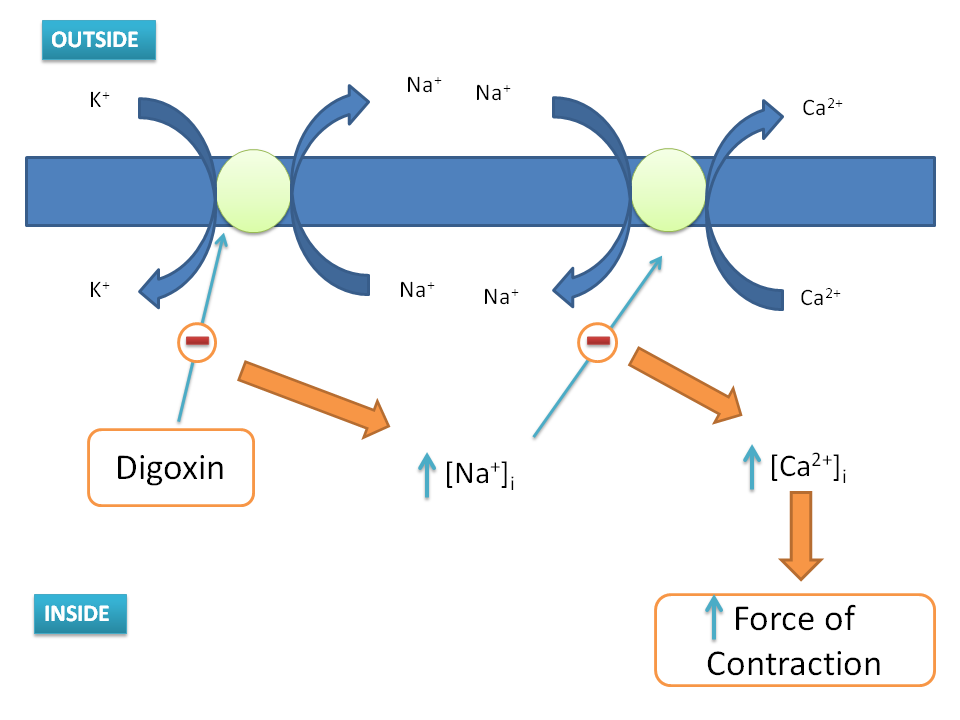
Digoxin is a cardiac glycoside that acts as ionotropic agent that increases the force of contraction of the heart hence indicated for heart failure.
Digoxin inhibits Na+/K+-ATPase pump on the heart by binding to the potassium binding site. This results in increase intracellular Na+ levels. This in turn inactivates Na+/Ca2+ - exchange pump leading to increased intracellular calcium levels in the heart. These calcium levels are then stored in sarcoplasmic reticulum and when cell is depolarised a large amount of calcium is effluxes from SR resulting in increased force of contraction.
Digoxin toxicity can induce cardiac arrhythmias by several mechanisms.The same mechanism which is responsible for increase in the force of contraction may also responsible for ventricular arrhythmias.
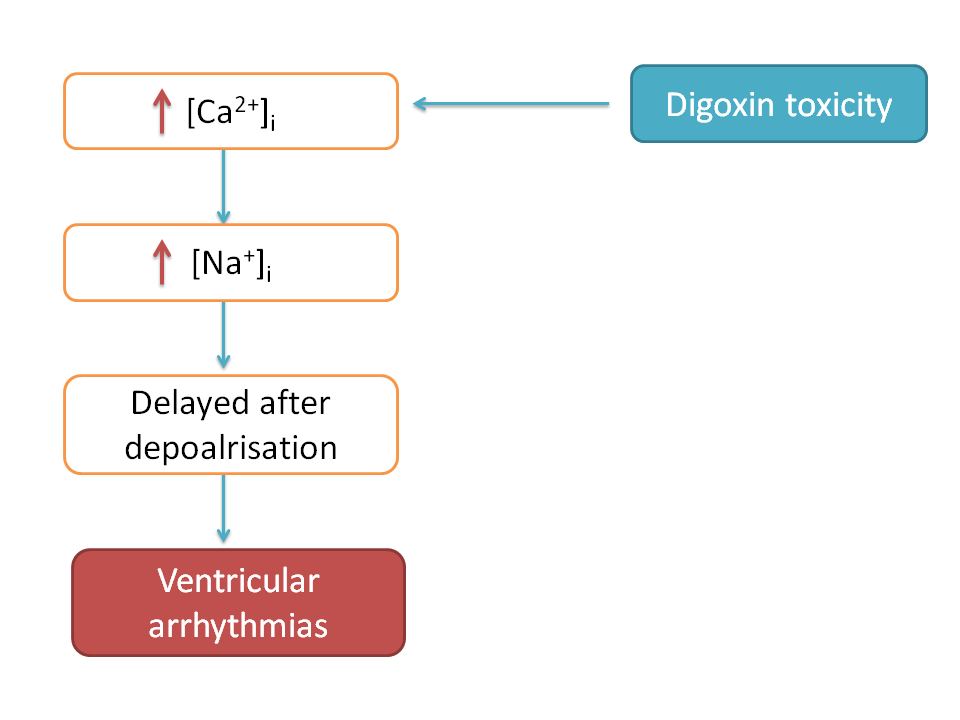
Normal dose of digoxin may not immediately produce ventricular arrhythmias but at a toxic dose digoxin abnormally increases intracellular calcium, which in turn abnormally increases intracellular Na+ by acting on Na+/Ca2+ - exchange pump.
These abnormally raised Na+ levels then may cause depolarisation of membrane even after completion of normal depolarisation leading to an extra beat. This is called delayed after depolarisation. This can be sometimes observed as increase in QT interval in ECG.
Now let’s see another mechanism of cardiac toxicity produced by digoxin.
Digoxin also increases vagal activity leading decreased AV conduction thereby suppresses atrial fibrillation.
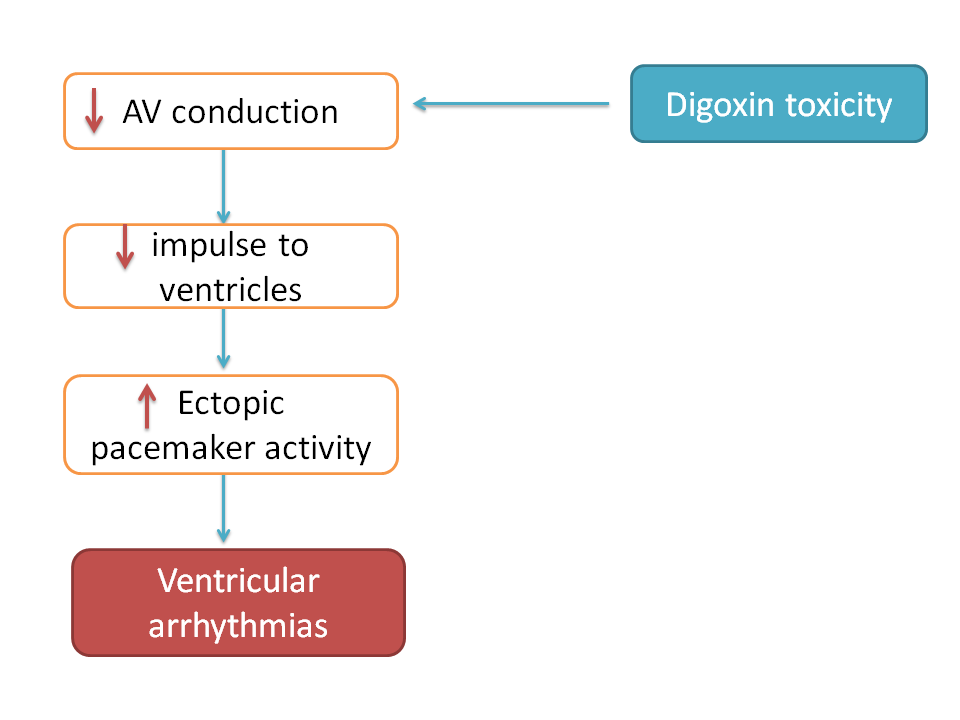
Since it decreases AV conduction ventricles get less impulse raising the ectopic pacemaker activity of ventricles making the later to generate their own impulses.
This condition may lead to ventricular arrhythmias which are fatal and immediately treated by lidocaine.